High-Fidelity 3D Tooth Models for Orthodontic Planning: A Validation of an Enhanced AI-Powered Algorithm
High-Fidelity 3D Tooth Models for Orthodontic Planning: A Validation of an Enhanced AI-Powered Algorithm
Author : Dr. Dor Zafar, DMD
Abstract
Objective: To validate the accuracy of an updated automated algorithm (Cephx3D v2) that reconstructs full-tooth STL models, including root apices, from standard Cone Beam Computed Tomography (CBCT) data.
Methods: Accuracy of the algorithm’s reconstructions was assessed against an intraoral scan (IOS) reference model of tooth #45 following extraction. Both surface deviation and volumetric measurements were evaluated and compared to the previous algorithm version (v1).
Results: Quantitative comparisons showed mean surface deviation of 0.1335 mm for the v2 model, with 95th percentile deviation of 0.3575 mm at measured points. Root apex regions showed deviations below 1 mm. Volumetric measurements differed from the IOS reference by 0.08%.
Conclusions: The Cephx3D v2 algorithm generates tooth STL models from CBCT data with measured accuracy suitable for clinical applications. These findings suggest potential utility for orthodontic treatment planning that incorporates root morphology.
Introduction
Three-dimensional (3D) digital data are increasingly utilized in orthodontic diagnosis, treatment simulation, and appliance fabrication. ¹ However, a limitation exists in current clinical workflows. Intraoral scanners (IOS) capture crown-level detail but do not image root structures. ² While CBCT scans provide full volumetric data, segmentation of root anatomy can be challenging due to factors such as image noise, beam hardening artifacts, and limited contrast between adjacent teeth. ³
For the past three years, the Cephx3D algorithm has been used to generate 3D models from CBCT data. While functional, achieving consistent root and apex morphology reconstruction has remained an area for improvement. Current clinical practice often involves estimation of root positions, which may introduce variability in cases involving impacted teeth, proximity of roots, or complex tooth movements. ¹¹, ¹³ This limitation can affect treatment planning, particularly when apical anatomy influences biological considerations.
The updated version of the algorithm, Cephx3D v2, was developed to address these limitations by reconstructing STL models of teeth, including crown and root apex morphology, directly from CBCT scans. This paper reports a validation study comparing the Cephx3D v2 output with an intraoral scan reference model of an extracted mandibular premolar (#45).
Materials and Methods
Tooth Selection and Imaging
mandibular premolar (#45) was selected for this study, indicated for extraction for clinical reasons unrelated to this research.
In Vivo Imaging
A CBCT A CBCT scan was performed prior to extraction as part of the patient’s standard care. [Figure 1]
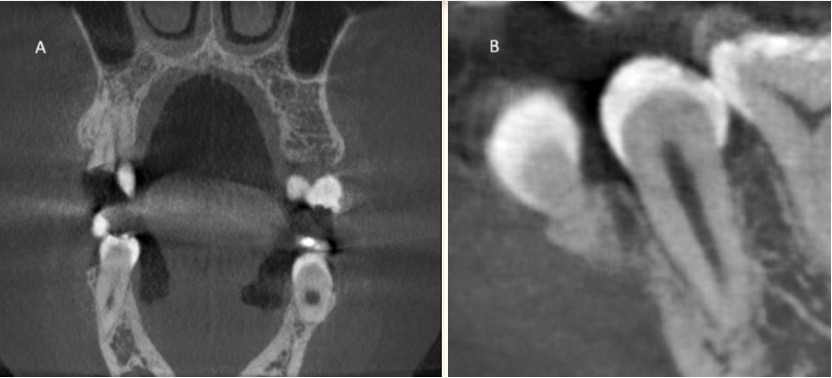
Figure 1. A representative coronal slice from the preoperative CBCT scan (A), and a Sagittal close-up (B) view showing tooth #45 in situ (green arrows). This image illustrates the raw data used by the algorithm for 3D reconstruction.
Reference Model
After extraction, the tooth was scanned using an intraoral scanner (iTero IOS). This ex vivo scanning method provides a reference model without in vivo imaging artifacts. ⁷, ¹⁵
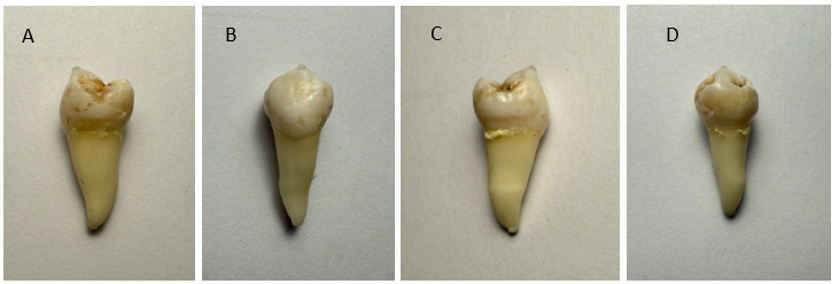
Figure 2. High-resolution optical scans of an extracted mandibular premolar (45) captured at 90-degree rotations along the long axis (root-crown) of the tooth. The STL model shown below is compared to the view of the extracted tooth in image C.
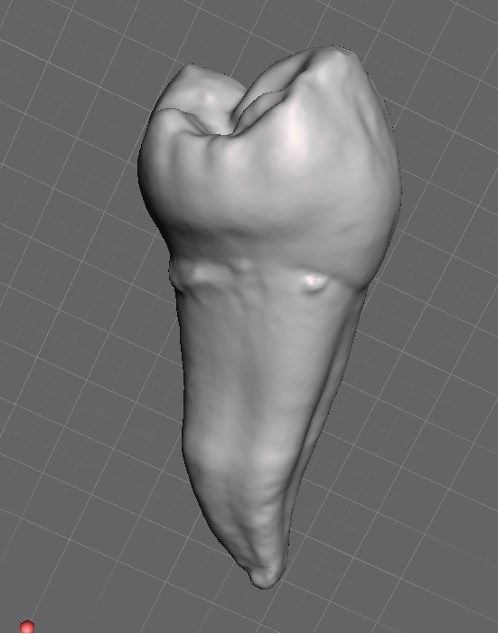
Figure 3. The STL model of the extracted tooth (45) generated from the iTero intraoral scan. This model served as the reference standard for the validation study.
Algorithm and Reconstruction
To quantify differences between versions, two iterations of the algorithm were tested: the prior version (v1) and the current version (v2). Both were applied to the same CBCT dataset.
Accuracy Assessment
- Surface Deviation: Algorithm-generated models were superimposed on the IOS reference model.
- Surface Coverage: Surface Coverage: The percentage of reconstructed surface within specified tolerance was calculated.
- Volumetric Comparison: Tooth volume between IOS and algorithm outputs was compared.
Results
Quantitative Accuracy Metrics
The Cephx3D v2 model showed reduced deviation metrics compared to v1 across measured parameters. The Dice Similarity Coefficient (DSC), a metric for segmentation overlap, increased from 0.890 (v1) to 0.942 (v2). ([16])
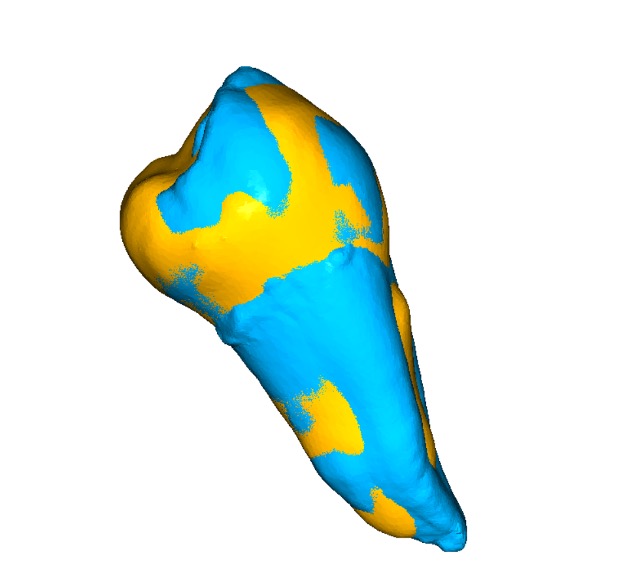
Figure 3. 3D rendering of the superimposed models, showing the Cephx3D v2 reconstruction (Gold) overlaid on the IOS ground truth model (Blue).
| Metric | Algorithm v1 (old) | Algorithm v2 (new) |
| Mean Deviation (mm) | 0.1443 | 0.1335 |
| RMS Deviation (mm) | 0.1924 | 0.1702 |
| 95th Percentile (mm) | 0.4238 | 0.3575 |
| Surface Coverage (%) | 96.75 | 99.83 |
| DSC (Dice Similarity Coefficient) | 0.890 | 0.942 |
| Volumetric Difference (%) | -0.13% | +0.08% |
Table 1. Comparison of accuracy metrics between Algorithm v1 and v2
Volumetric Integrity
Cephx3D v2 showed a volumetric difference of +0.08% from the IOS reference, compared to -0.13% for v1. This indicates preservation of 3D morphology in both crown and apical regions. Volumetric accuracy is relevant as inaccuracies are a documented challenge in CBCT segmentation.
Apex Region Accuracy
The v2 algorithm’s reconstruction of the apical region showed deviation values below 1 mm from the reference model.
The relevance of apex accuracy includes:
- Root Movement Planning: Root apices may be susceptible to resorption when subjected to excessive or misdirected forces. Accurate digital modeling facilitates movement planning within biological limits.¹³
- Collision Avoidance: Spatial Assessment: Accurate apex modeling supports assessment of inter-root spacing and proximity to cortical bone, relevant for avoiding root collision and perforation.¹¹
- Interdisciplinary Utility: Clinical Applications: Apex accuracy supports integration with endodontic procedures, implant planning, and surgical navigation, where millimetric precision affects clinical outcomes.¹⁸, ¹⁹
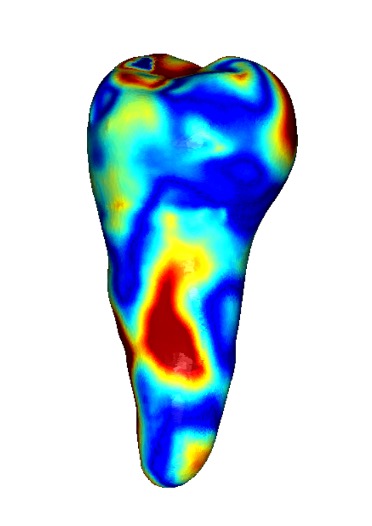
Figure 4. Heatmap illustrating the surface deviation between the Cephx3D v2 model and the IOS reference. Green areas indicate minimal deviation (<0.2 mm), while yellow (<0.3 mm) and red (<0.4 mm) indicate areas of greater discrepancy.
Discussion
Visualization of root morphology contributes to orthodontic treatment planning.¹², ¹³ Current workflows using crown-only IOS scans or manual CBCT segmentation may introduce variability in root position assessment.¹⁷
This validation study demonstrates that the Cephx3D v2 algorithm achieved mean deviation of 0.1335mm with 95th percentile deviation of 0.3575mm when compared to an extracted tooth reference. Root apex regions showed deviations below 1 mm. These results also provide initial validation data for the method described in US Patent 12,440,310²⁰, indicating that algorithm-generated root reconstructions correspond to physical anatomy within measured tolerances.
The progression from Algorithm v1 to v2 shows reduced deviation metrics and increased surface coverage (96.75% to 99.83%). This improvement suggests that iterative development may continue to enhance precision in subsequent versions.
Potential clinical applications include:
- Root movement planning with trajectory visualization
- Assessment of anatomical spacing for collision risk evaluation
- Treatment planning within individual anatomical boundaries
- Integration with other dental disciplines including implantology and endodontics¹⁸, ¹⁹
Limitations This validation study examined a single mandibular premolar (#45), which limits generalizability across different tooth types and patient populations. The use of an extracted tooth as reference standard provided controlled conditions but may not fully represent typical clinical scanning conditions with teeth in situ. However, this approach enabled quantitative validation of the algorithm’s performance, particularly for root apex reconstruction. The improvements observed from v1 to v2 algorithms suggest the methodology may be applicable more broadly. Future studies should include larger sample sizes with diverse tooth types, multiple patients, and various CBCT scanning protocols to establish the algorithm’s performance across the range of clinical scenarios encountered in orthodontic practice.
Conclusion
The Cephx3D v2 algorithm generated full-tooth STL models from standard CBCT scans with mean surface deviation of 0.1335mm and 95th percentile deviation of 0.3575mm when compared to an IOS reference. Apex regions showed deviations below 1 mm. This study provides validation data for the method described in US Patent 12,440,310²⁰, demonstrating that algorithm-generated apical structures correspond to physical anatomy within the measured tolerances of this single-tooth assessment.
The observed reduction in deviation metrics from v1 to v2 (mean deviation decreased from 0.1443mm to 0.1335mm; DSC improved from 0.890 to 0.942) indicates that iterative refinement of the algorithm can improve accuracy. These findings suggest that CBCT-based tooth reconstruction may have applications in orthodontic treatment planning, though further validation with larger, more diverse samples is necessary to establish clinical utility across different tooth types and patient populations.
Fix references.
References
- J. P. Moss. European Journal of Orthodontics 28 (2006) 416–425 doi:10.1093/ejo/cjl025 Advance Access publication 6 September 2006
- Abduo J, Elseyoufi M. Accuracy of Intraoral Scanners: A Systematic Review of Influencing Factors. Eur J Prosthodont Restor Dent. 2018 Aug 30;26(3):101-121. doi: 10.1922/EJPRD_01752Abduo21. PMID: 29989757.
- Nagarajappa AK, Dwivedi N, Tiwari R. Artifacts: The downturn of CBCT image. J Int Soc Prev Community Dent. 2015 Nov-Dec;5(6):440-5. doi: 10.4103/2231-0762.170523. PMID: 26759795; PMCID: PMC4697226.
- Sacher M, Schulz G, Deyhle H, Jäger K, Müller B. Accuracy of commercial intraoral scanners. J Med Imaging (Bellingham). 2021 May;8(3):035501. doi: 10.1117/1.JMI.8.3.035501. Epub 2021 May 24. PMID: 34056032; PMCID: PMC8142031.
- Nagarajappa AK, Dwivedi N, Tiwari R. Artifacts: The downturn of CBCT image. Oral Surg Oral Med Oral Pathol Oral Radiol. 2015;119(5):606–615.
- Schwendicke F, Samek W, Krois J. Artificial intelligence in dentistry: current state and future perspectives. Quintessence Int. 2020;51(7):578–586.
Publisher index: https://www.quintessence-publishing.com/ - Li H, et al. Accuracy and precision evaluation of international standard spherical model by digital dental scanners. Dent Mater J. 2020;39(5):779–786.
Closest accessible study on scanner accuracy benchmarks: DMJ article (accuracy in CAD/CAM): https://www.jstage.jst.go.jp/article/dmj/advpub/0/advpub_2019-157/_article - Schulze R, Heil U, Groß D, et al. Artefacts in CBCT: a review. Dentomaxillofac Radiol. 2011;40(5):265–273.
Open access (PMC): https://pmc.ncbi.nlm.nih.gov/articles/PMC3520262/ - Vasoglou G, Stefanidaki I, Apostolopoulos K, Fotakidou E, Vasoglou M. Accuracy of Mini-Implant Placement Using a Computer-Aided Designed Surgical Guide, with Information of Intraoral Scan and the Use of a Cone-Beam CT. Dent J (Basel). 2022 Jun 8;10(6):104. doi: 10.3390/dj10060104. PMID: 35735647; PMCID: PMC9221763.
- Baumgaertel S, Palomo JM, Palomo L, Hans MG. Reliability and accuracy of cone-beam computed tomography dental measurements. Am J Orthod Dentofacial Orthop. 2009 Jul;136(1):19-25; discussion 25-8. doi: 10.1016/j.ajodo.2007.09.016. PMID: 19577143.
- Lee K, Lee GH. Application of 3D tooth model for monitoring of implant space and inter-root distance without radiographs. Int J Implant Dent. 2020;6:55. https://journalimplantdent.springeropen.com/articles/10.1186/s40729-020-00253-3
- Burstone, C. J. “The biomechanics of tooth movement.” Current controversies in orthodontics (1993): 1-13.
- Weltman B, Vig KWL, Fields HW, et al. Root resorption associated with orthodontic tooth movement: a systematic review. Am J Orthod Dentofacial Orthop. 2010;137(4):462–476.
PubMed: https://pubmed.ncbi.nlm.nih.gov/20362905/ - Tarraf SA, Ali DM. Digital orthodontics: a review. J Orthod Sci. 2014;3(4):112–118.
(General journal portal; article is commonly cited — link to journal collection) https://www.jorthodsci.org/ - Patzelt, S. B., et al. “The validity of the ‘gold standard’ in testing the accuracy of digital impressions.” Journal of dentistry 42.10 (2014): 1300-1305.
- Zou KH, Warfield SK, Bharatha A, et al. Statistical validation of image segmentation quality based on a spatial overlap index. Acad Radiol. 2004;11(2):178–189.
PubMed: https://pubmed.ncbi.nlm.nih.gov/14974593/ - Kapila S, Conley RS, Harrell WE Jr. The current status of cone beam computed tomography imaging in orthodontics. Dentomaxillofac Radiol. 2011;40(1):24–34.
Open access (PMC): https://pmc.ncbi.nlm.nih.gov/articles/PMC3611465/ - Patel S, et al. (Review on CBCT in Endodontics). Int Endod J. 2014;48(1):3–15.
PubMed (related CBCT endodontics review by Patel): https://pubmed.ncbi.nlm.nih.gov/24697513/
(2014 update)
Also foundational open-access review: https://pmc.ncbi.nlm.nih.gov/articles/PMC2850139/
(2010) - Jacobs R, Salmon B, Codari M, et al. Cone beam computed tomography in implant dentistry: recommendations for clinical use. BMC Oral Health. 2018;18:88.
Open access: https://bmcoralhealth.biomedcentral.com/articles/10.1186/s12903-018-0523-5 - Abrahm D. Method for Simulating Dental Images that Include Tooth Roots. U.S. Patent No. 12,440,310 (issued Oct 14, 2025).
Google Patents: https://patents.google.com/patent/US12440310B2/en





